The Truth About Probiotics: Why Most Don’t Work
The Probiotic Marketing Trap
Probiotics have exploded into a billion-dollar industry, promising everything from weight loss to better skin and “balanced hormones.”
From glossy supplement labels to influencer posts about kombucha, it’s easy to believe a daily pill will fix your gut.
But here’s the truth: most probiotic supplements don’t work — at least not the way the marketing makes it seem.
A huge number of probiotic products are:
Formulated with strains that don’t match what the research supports
Poorly absorbed because they die in the stomach
Not tested in humans at all
Sold at high doses that don’t mean much without context
So if you’ve tried probiotics and felt zero difference, you're not alone.
It’s not your body that’s the problem — it’s likely the product.
Why Most Probiotics Fail
Let’s start with the basics: probiotics are live microorganisms that are meant to confer health benefits when consumed in adequate amounts.
But many supplements fail on that front before they even reach your gut.
A 2016 study published in Frontiers in Microbiology tested 25 commercial probiotic products. It found that only a small number matched their label claims — and even fewer delivered live organisms to the gut.
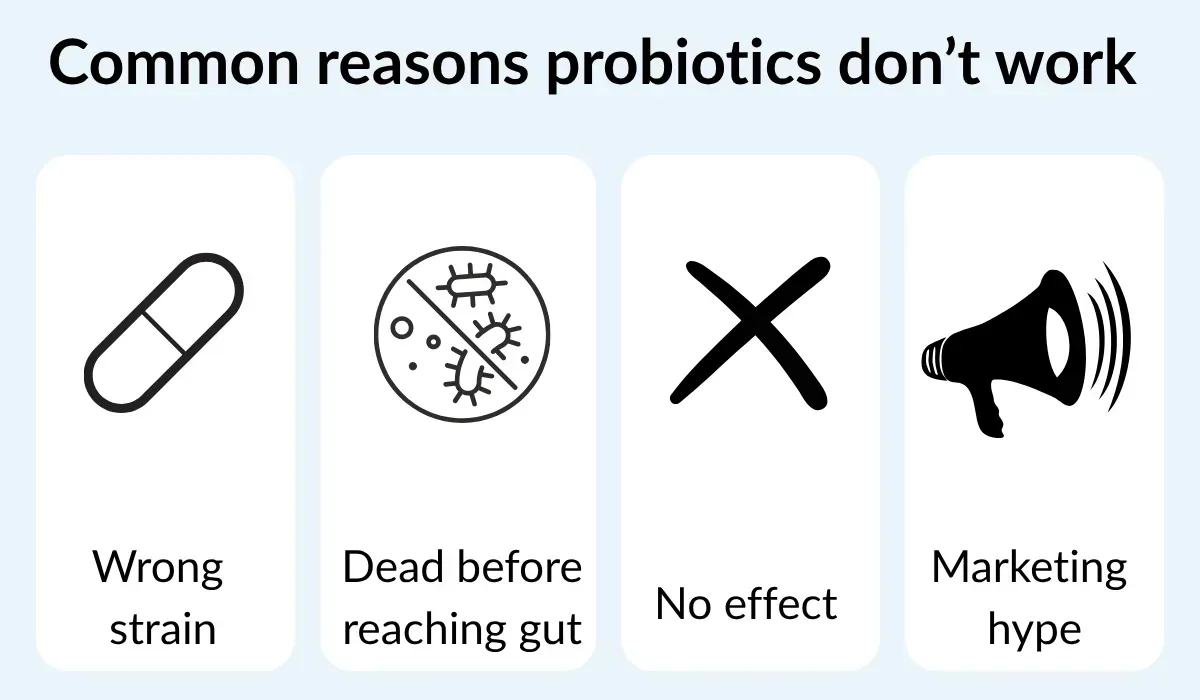
Common reasons probiotic supplements fail:
Poor survivability through stomach acid
Wrong or unproven strains
No supportive environment (like prebiotics or a healthy gut lining)
Low-quality control or incorrect labeling
The 3 Criteria That Make a Probiotic Effective
Leading researchers like Dr. Mahmoud Ghannoum (Case Western Reserve University) and Dr. Megan Rossi (The Gut Health Doctor) agree that effective probiotics must meet these three criteria:
1. Strain-specific effects
For example, Lactobacillus rhamnosus GG has been shown to support diarrhea recovery and immune function in multiple clinical studies (Szajewska et al., 2016). But Lactobacillus rhamnosus GR-1, a closely related strain, supports vaginal microbiota — not digestion (Reid et al., 2001).
2. Survivability through the GI tract
Most bacteria die in stomach acid. Probiotic strains need to survive that journey, often via delayed-release capsules or microencapsulation. This has been shown to improve outcomes in clinical settings (McFarland, 2015).
3. Backed by peer-reviewed human studies
You want research done on actual people — ideally those with symptoms or characteristics similar to your own.
Probiotic Strains That Actually Work
Some strains have been well studied in human trials and consistently show benefits. Here are five of the most effective:
🦠 Lactobacillus rhamnosus GG
✅ Supports: Diarrhea recovery, immune function
🔬 Szajewska et al., 2016 – J Pediatr Gastroenterol Nutr
🦠 Bifidobacterium infantis 35624
✅ Supports: IBS symptoms like bloating, cramping, and irregular bowel movements
🔬 Whorwell et al., 2006 – Gut
🦠 Saccharomyces boulardii
✅ Supports: Recovery from antibiotic-associated and traveler’s diarrhea
🔬 Kelesidis et al., 2012 – Therap Adv Gastroenterol
🦠 Lactobacillus reuteri DSM 17938
✅ Supports: Constipation, colic relief, oral and dental health
🔬 Savino et al., 2007 – Pediatrics
🦠 Bacillus coagulans GBI-30 6086
✅ Supports: Gas, bloating, and general digestive discomfort
🔬 Kalman et al., 2009 – Food Microbiol
Even with these strains, context matters. They work best in an environment where inflammation is under control and the gut lining is healthy.
Food Sources vs Supplements: Which Is Better?

You don’t always need a supplement.
Fermented foods have been shown to naturally increase microbiome diversity, reduce inflammation, and provide additional nutrients and enzymes that capsules lack.
According to Dr. Megan Rossi, and in line with a 2021 clinical trial from Stanford University, participants who ate a diet rich in fermented foods (like kefir and sauerkraut) saw:
Increased microbial diversity
Decreased markers of chronic inflammation
Top probiotic-rich foods:
Live-culture yogurt
Kefir
Sauerkraut (raw)
Kimchi
Miso
Tempeh
Kombucha (watch the sugar)
Supplements are sometimes helpful, but for most women, food-first works better and lasts longer.
How to Take Probiotics for Maximum Benefit
If you’re going to use a supplement, use it smartly:
✅ Take with food — This improves survivability through the stomach (Tompkins et al., 2011)
✅ Include fiber — Probiotics need fuel (prebiotics) to thrive
✅ Store correctly — Some need refrigeration; heat kills them
✅ Cycle and rotate — Don’t stay on the same strain forever
And always remember: probiotics are not a magic fix — they’re one tool in a broader healing process.
Red Flags in Probiotic Marketing
Here’s what to watch out for:
🚩 "Billions of CFUs!" — Quantity means nothing without quality and survivability.
🚩 No strain names listed — If a product says “Lactobacillus” without the full strain ID, it’s a red flag.
🚩 “Clinically proven” without citations — If there are no references, assume there’s no real research.
🚩 “Fixes everything” promises — If it claims to solve bloating, anxiety, fatigue, and weight gain all at once, it’s probably overhyped.
When Probiotics Aren’t the Answer
Here’s the part few brands will admit:
if your gut lining is inflamed or leaky, probiotics alone won’t help.
That’s like planting seeds on dry, cracked soil.
As Dr. Mahmoud Ghannoum explains in Total Gut Balance, restoring gut health requires:
Reducing inflammation
Supporting the gut lining
Rebalancing both bacteria and fungi (the mycobiome)
This step is missing in almost all “probiotic protocols.”
A Better Approach: Heal Before You Add
Before reaching for another probiotic supplement, ask:
“Is my gut environment ready to receive them?”
That’s why I created the 28-Day Gut Reset.
It’s a short, food-based protocol that:
Heals the gut lining first
Eliminates irritants and inflammation
Reintroduces probiotic-rich foods naturally
Rebuilds diversity with real food
And yes — there are probiotics included.
But not in capsule form.
They're in the fermented, whole foods you eat — supported by a plan that truly makes space for them to work.
Final Thoughts: Are Probiotic Supplements Worth It?
The bottom line:
Yes, some probiotics work — but only when they’re the right strain, taken in the right way, and supported by a healthy gut environment.
No, most off-the-shelf probiotics are not effective.
You don’t need to waste money on a supplement that won’t make a dent in your symptoms.
Instead, start where healing really begins: by fixing the foundation.
✅ Want to finally feel a difference?

Try the 28-Day Gut Reset — a step-by-step food-based plan to repair your gut lining and support real digestive health.
📚 References
Gueimonde M, et al. (2016). Evaluation of Probiotic Strains in Commercial Products. Frontiers in Microbiology, 7:737. https://doi.org/10.3389/fmicb.2016.00737
Sanders ME, et al. (2013). Probiotics and prebiotics in intestinal health and disease. Gut Microbes.
Reid G, et al. (2001). Probiotic Lactobacillus dose required to restore and maintain a normal vaginal flora. FEMS Immunol Med Microbiol, 32(1):37–41.
Szajewska H, et al. (2016). Probiotic use in acute gastroenteritis in children. J Pediatr Gastroenterol Nutr, 62(3):495–506.
Whorwell PJ, et al. (2006). Efficacy of an encapsulated probiotic Bifidobacterium infantis 35624 in IBS. Gut, 55(7):913–920.
Kelesidis T, et al. (2012). Saccharomyces boulardii: A review of current evidence for its use in clinical practice. Therap Adv Gastroenterol, 5(2):111–125.
Savino F, et al. (2007). Lactobacillus reuteri DSM 17938 in infantile colic. Pediatrics, 119(1):e124–e130.
Kalman DS, et al. (2009). Effect of Bacillus coagulans GBI-30, 6086 on gastrointestinal symptoms. Food Microbiology, 26(8):677–683.
Rossi M. (2019). Eat Yourself Healthy. Penguin Life.
Wastyk HC, et al. (2021). Gut-microbiota-targeted diets modulate human immune status. Cell, 184(16):4137–4153.e14.
Tompkins TA, et al. (2011). Effect of ingestion of probiotic Lactobacillus and Bifidobacterium strains on gastrointestinal symptoms. Benef Microbes, 2(1):57–66.
Ghannoum MA. (2019). Total Gut Balance. Hay House.
Sunel Visser
Sunel’s journey with gut health began while living in Thailand, when she developed severe digestive issues.
Determined to find a natural, lasting solution — without antibiotics or 'cop out' medical labels — she dedicated herself to deep research and experimentation.
The result was a transformative protocol that restored her digestive health, stabilized her weight fluctuations, and improved her immune system and overall quality of life - since 2014.
Sunel holds a degree in Sport Science, an Honours degree in Psychology, is a Certified Personal Trainer, Certified Strength and Conditioning Specialist, and has an Advanced Certificate in Nutritional Counseling.
Quick links
Contact
sunel@sunelvfitness.com
+27 84 558 7015